More than 180 participants gathered in Barcelona last 16 November 2017 for the 6th Meeting of the EAU Section of Urological Imaging (ESUI17). With the high attendance and enthusiastic discussions, ESUI17 demonstrated the sustained interest for urological imaging and its profound impact on the treatment of uro-oncological diseases.
Speaker Prof. Monique Roobol (NL) brought forward some thought-provoking arguments to this year’s meeting in her lecture “What is an acceptable false negative rate in the detection of prostate cancer?”
Are we doing the right thing in debating about how to increase the detection rate of prostate cancer (PCa) or should we accept to overlook some cancers? In a survey by Rashid Khalid Sayvid et al., 65% of patients would accept a false negative rate of 5-20%, while among urologists the figure is even higher at 78%, according to Prof. Roobol. In the ERSPC study after 15 years of follow-up, csPCa incidience, rate of metastasis and mortality were very low in men who had a negative sextant biopsy (re-tested every four years in case of a negative sextant biopsy, Photo slide 11?
The fact that a sextant biopsy, which is no longer up-to-date, was used as the detection method for PCa made this data even more thought-provoking. She concluded that we should all realize that the risk of actually missing the diagnosis of a potentially metastatic or life-threatening prostate cancer might be low. With this in mind, the results of the PROMIS trial with a NPV for mpMRI of 76% for Gleason >= 3+4 could be seen with more optimism.
Besides the false negative rate of mpMRI, PIRADS 3 lesions represent a difficult approach for decision-making whether to biopsy or not, due to its inaccurate detection of csPCA. Biomarkers might help enhanced ultrasound methods such as micro-ultrasound which might further define PIRADS 3 lesions to increase the positive predictive value.
Anyhow, as stated by Prof. Hadashik, the amount of PIRADS 3 lesions defined by the radiologists should definitely be lowered as a clear statement of whether to biopsy or not. To resolve this issue, the key factors are training and expertise in MRI reading.
Last but not least, there is no doubt that inter-disciplinarily is a requirement for good patient care and this was demonstrated from various viewpoints, such as those of radiologists, pathologists and urologists.

Best abstract
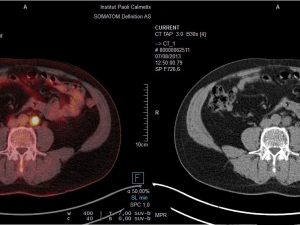
More than 20 abstracts have been submitted for this year’s ESUI meeting with six posters selected for the oral presentation. Dr. Del Vecchio won the top award (sponsored by Exact Imaging). Del Vecchio came all the way from Woolloongabba, Australia to Barcelona to present her research regarding the distinction between malignant and clear cell renal cancers, and indolent subtypes with the use of MR spectroscopy. This technique might potentially identify indolent/SRM from those that are aggressive and life-threatening.
We hope to see you at the 7th Meeting of the EAU Section of Urological Imaging (ESUI18) on 8 November 2018 in Amsterdam for another interesting program on urological imaging!